There are many treatment options for cancer today, yet it continues to be a major health problem, killing hundreds of thousands of people in the US each year. While conventional therapies like chemo and radiation have successfully extended survival rates, they don’t necessarily work for all patients, especially those with late-stage or rare cancers. As a result, more advanced treatments and diagnostic methods are being sought after to stem the cancer death toll.
One research area that shows great promise for cancer treatment is epigenetics. Several studies have shown that many human cancers possess epigenetic abnormalities, as well as genetic alterations. Essentially, these two factors work in collaboration to initiate and promote the disease. However, because epigenetic modifiers do not permanently alter DNA and are potentially reversible, they are promising targets for various cancer therapies.
In a recent study, researchers from the Mayo Clinic’s Center for Individualized Medicine have identified epigenetic marks associated with a rare bone marrow cancer that appears to be rapidly driving the disease. This cancer, known as ASXL1-mutant chronic myelomonocytic leukemia, is caused by a genetic mutation. Although, the underlying epigenetic changes are responsible for activating the ASXL1 gene, causing a more aggressive form of myeloid leukemia.
“The epigenome in patients with these ASXL1 gene mutations is changed in a way that allows the cancer cells to switch on genes that are detrimental to the patients,” said lead research author and hematologist Dr. Moritz Binder. “These epigenetic changes don’t affect the DNA blueprint itself. It affects how the blueprint is read — which pages to read and which pages not to read.”
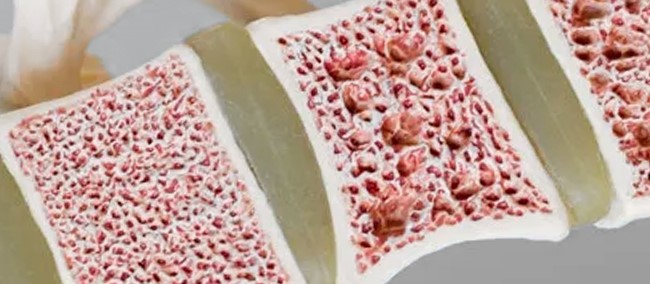
Chronic myelomonocytic leukemia (CMML) is an uncommon form of cancer that usually affects older adults. It begins when bone marrow stem cells mutate, resulting in abnormal blood cell production. As this disease progresses, the bone marrow becomes full of defective cells and can’t make enough normal ones. Eventually, the lack of sufficient blood cells causes problems like anemia and infections that don’t heal.
Close to 40% of CMML patients carry ASXL1 mutations. Yet, most do not fare well or find relief from current treatments. Dr. Binder and his team hoped to determine what was distinctive about this mutation by examining the molecular mechanisms underlying the disease.
In the study, the researchers chose to survey the epigenetic landscape of CMML, performing an extensive multi-omics interrogation to assess gene expression levels and chromatin remodeling directly related to ASXL1. Their analysis was determined by evaluating and comparing samples of bone marrow mononuclear cells obtained from 16 CMML patients, half of which had the mutation.
From the samples collected, the team used a variety of high-throughput sequencing methods, including DNA targeted next-generation sequencing (NGS), whole transcriptome RNA-sequencing (RNA-seq), chromatin immunoprecipitation sequencing (ChIP-Seq), immunoprecipitation of DNA hydroxymethyl and methyl residues (DIP-seq), and Assay for Transposase-Accessible Chromatin using sequencing (ATAC-seq).
“This allowed us to perform modeling to draw inference about the effect of epigenetic changes in isolation and in concert on leukemogenic gene expression in ASXL1-mutant chronic myelomonocytic leukemia,” said Dr. Binder.
Their results revealed that ASXL1 mutations are connected with the overexpression of important leukemogenic driver genes. In particular, they saw a reduction in repressive histone methylation and a rise in permissive histone methylation and acetylation in promoter regions.
Because the data implies that these regulatory mechanisms only appear in patients carrying the mutation, it can be used as a comprehensive map of the chromatin landscape for ASXL-mutant CMML. Moreover, the findings lay the groundwork for developing innovative targeted therapeutic strategies for patients with this disease. The team plans to follow up on their study with early phase clinical trials sometime in the future.
Dr. Binder commented, “Our study is the basis for ongoing work to further explore ways to target these patient-specific regulatory elements with novel small-molecule drugs. With this approach, we hope to restore normal gene expression, or at least treat the cancer cells in a new way to overcome the detrimental effect of ASXL1 mutations.”
Source: M. Binder, et al. Oncogenic gene expression and epigenetic remodeling of cis-regulatory elements in ASXL1-mutant chronic myelomonocytic leukemia. Nature Communications, March 17, 2022.
Reference: Susan Murphy, Mayo Clinic discovery in bone marrow cancer points to potential drug targets. May Clinic, March 17, 2022.

