Most people know antibodies as the “warriors” of our immune system, helping us fight off invading pathogens. But not all antibodies are made for this purpose. Some perform necessary maintenance functions, such as clearing the blood of wastes like oxidized LDL cholesterol. These, too, are just as vital for keeping us safe and healthy. Understanding how we acquire antibodies of any type is of interest to scientists because irregularities in our ability to produce them could lead to disease development.
Deciphering variations in cells that create different antibodies entails examining their distinct epigenetic landscapes. That’s because all cells in the body share the same genetic code. It’s the specific chemical tags or epigenetic modifications which attach to the DNA, turning “on and off” certain genes that make cells unique. If you can identify a cell’s epigenetic signature, you can then determine when abnormalities occur.
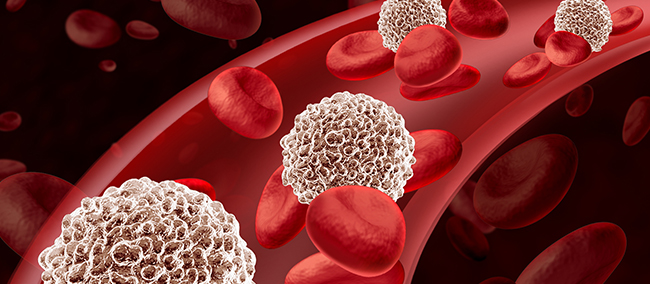
In a recent paper published in Nature Communication, a team of researchers conducted a study to analyze the epigenetic differences that determine the fate of cells that produce antibodies. Given the crucial role that DNA methylation plays in controlling gene expression, heredity, and cellular state, they conducted a genome-wide study of cytosine methylation for two distinct sub-lineages of B lymphocytes (B cells) – the specialized white blood cells that make antibodies.
The majority of B-cells in the body are short-lived, recirculating cells classified as B2 cells. They belong to the adaptive immune system and create antibodies in response to foreign substances. A smaller subset of B cells, known as B1 cells, live longer and self-renew, producing natural antibodies as part of the body’s innate immunity.
According to the study’s first author, Vinay Mahajan, MD, PhD, and pathology instructor at the Ragon Institute of MGH, MIT, and Harvard, B cell outcome is determined by epigenetic modifications made possible via DNA methyltransferases (DNMTs), specifically DNMT3A. He said, “Genetic studies in humans link the genomic regions with these markers to a variety of immune-mediated disorders.”
DNA is made up of 4 main bases: cytosine, adenine, guanine, and thymine. Generally, DNA methylation occurs predominantly on cytosine followed by guanine residues and is known as CpG methylation. The main function of DNA methylation is to suppress gene expression, and DNMTs are the enzymes that bring about methylation at CpG sites. By assessing the CpG sites, the researchers were able to detect a set of unique regulatory elements within the B1 and B2 cells.
Once CpG methylation is added, it is permanent and will even pass on to replicated cells. However, in B cells, DNMT3A was continuously needed to maintain methylation. Disruption of this enzyme in B1 cells means epigenetic modification does not take place. The results lead to cells replicating out of control. This B1 cell abnormality is characteristic of Chronic lymphocytic leukemia (CLL) – a cancer of the blood and bone marrow.
“These unique B1 cells are vitally important to our ability to stay healthy,” says Shiv Pillai, MD, PhD and core member, Ragon Institute. “The antibodies they create help prevent clots and heart attacks. At the same time, understanding what genetic factors regulate them can help us better understand what happens when their regulation goes awry and leads to CLL and other diseases.”
Furthermore, this study illustrates the important role that DNA methyltransferases play in establishing epigenetic modifications in lineage-specific development. Without this epigenetic regulatory mechanism, cellular activity is corrupt and could lead to cell type-specific malignancy.
Source: Vinay S. et al. (2021). B1a and B2 cells are characterized by distinct CpG modification states at DNMT3A-maintained enhancers. Nature Communications.
Reference: Rachel Leeson. Epigenetic changes drive the fate of a B cell. Massachusetts General Hospital. May 14, 2021.

